5 Ways to Improve Sleep Quality with CGM and Your Glucose Levels

Sleep is where your body recovers, adapts, and rebuilds. For athletes, poor sleep isn’t just a nuisance—it directly impacts performance, recovery, and even long-term health. One of the most overlooked factors affecting sleep quality is glucose regulation.
Using a Continuous Glucose Monitor (CGM), athletes can uncover how diet, timing, and training influence nighttime glucose patterns, which in turn affect sleep depth, continuity, and next-day energy.
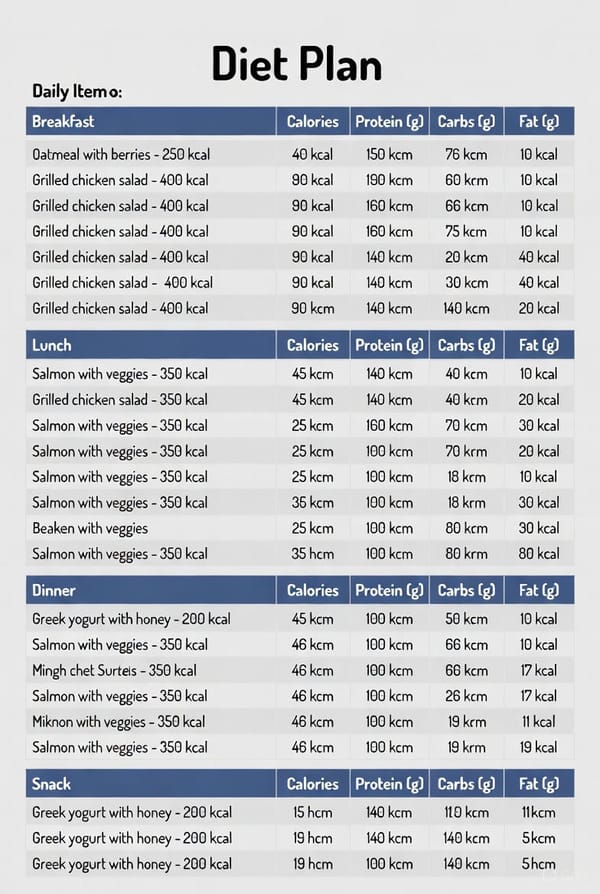
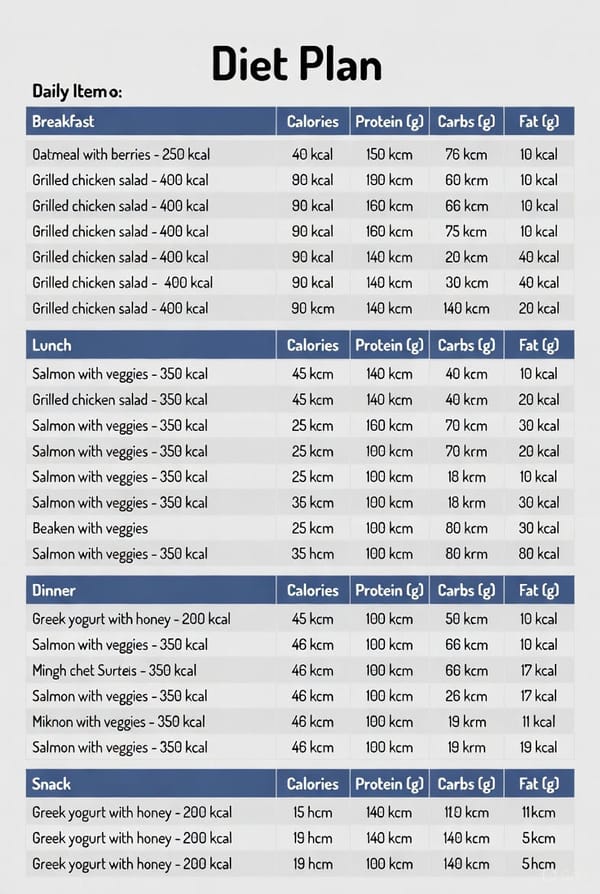
1. Stabilize Evening Glucose with Balanced Meals
Evening meals that are high in refined carbs or sugar can cause spikes followed by rapid drops in glucose, fragmenting sleep. Balancing protein, fiber, and healthy fats helps maintain a steady glucose curve overnight.
Tip: Include lean protein (chicken, fish, tofu), complex carbs (vegetables, legumes), and healthy fats (avocado, nuts) for optimal overnight stability.
2. Track Your Personal “Cut-Off Time”
Everyone metabolizes food differently. Some athletes tolerate late meals better than others. CGM allows you to find your personal cut-off time—the last window where eating doesn’t negatively impact your overnight glucose or sleep quality.
Tip: Use CGM data to test eating 2–4 hours before bed and compare glucose and sleep metrics.
3. Avoid High-Glycemic Foods Before Bed
Foods like white bread, sugary snacks, and even some fruit can spike glucose before sleep. This may lead to night waking, shallow sleep, and lower REM duration.
Tip: Check your CGM after eating suspect foods in the evening to see if they disturb your overnight glucose curve. Replace with low-glycemic alternatives like oats, nuts, or Greek yogurt.
Learn more about oatmeal and glucose response here:
👉 https://blog.supersapiens.com/continuous-glucose-monitoring-oatmeal/
4. Detect Hidden Stress Responses
Even without food, stress, late workouts, or high-intensity training in the evening can elevate glucose. CGM can reveal these hidden spikes, helping you take targeted action.
Tip: Pair your CGM data with relaxation routines such as stretching, meditation, or a light protein snack to balance glucose and cortisol levels.
5. Experiment and Review Next-Day Performance
The power of CGM lies in experimentation. By correlating glucose patterns with sleep metrics (deep sleep, REM, HRV), you can identify strategies that consistently improve recovery.
Tip: Keep a simple log of meals, training, sleep quality, and glucose readings. Over time, patterns emerge that let you optimize both sleep and performance.
Sleep Optimization Table Using CGM
| Strategy | How it Helps Glucose | Effect on Sleep | Actionable Step |
|---|---|---|---|
| Balanced Evening Meals | Prevents spikes and dips | Reduces night waking, improves deep sleep | Include protein, fiber, healthy fats |
| Identify Cut-Off Time | Avoids late-night glucose spikes | Supports smooth sleep onset | Test 2–4 hours pre-bed eating window |
| Avoid High-Glycemic Foods | Reduces sudden spikes | Minimizes sleep fragmentation | Swap sugary snacks for low-GI foods |
| Detect Stress Responses | Reveals hidden glucose elevations | Lowers cortisol-related sleep disruption | Pair CGM insights with relaxation routines |
| Experiment & Track | Finds personal patterns | Optimizes REM and HRV | Log meals, glucose, sleep, and performance |
Key Takeaway
Improving sleep isn’t just about going to bed earlier or cutting caffeine. Glucose stability is a powerful lever that affects every aspect of recovery and adaptation. By combining CGM insights with smart nutrition and timing, athletes can consistently improve sleep quality, recovery, and performance.