Ready to learn how sleep impacts your glucose levels and how your glucose levels impact your sleep?
Let’s get into it.
Research shows how sleep can affect your glucose levels, and how your glucose levels can affect your sleep. And both are critical to promote recovery and optimize performance.
How can you optimize recovery with sleep and glucose control?
There is no shortage of information on the benefits of sleep. Or on the potential adverse relationship between health and sleep deprivation. (For starters, there’s this TED talk on why we sleep by Russel Foster, the British Professor of Sleep Neuroscience.)
What’s much less studied? The impact of sleep on glucose. Or the effect of glucose levels on sleep quality.
Let’s start with the basics: Sleep, as you may be familiar with, is a homeostatically controlled behavioral state of reduced movement and sensory responsiveness. It’s also highly critical to both the cognitive and physiological function for all humans.
Recent studies show sleep actually regulates key molecular mechanisms, demonstrating that sleep plays an integral role in metabolic homeostasis.
The duration and quality of your sleep changes based on many environmental factors: light, exercise, and nutrition, to name a few. It’s also been shown to be influenced by genetic traits. So yes, sleep is complex. But, the need, the rationale, and the outcome of sleep all serve the important purpose of helping humans recover and get ready to perform. It’s been that way since the beginning of our evolution.
Poor sleep quality (waking up tired or feeling like your sleep was restless) is associated with difficulties in emotional and stress regulation as well as cognitive and physical performance.
Yes, sleep–good or bad–has its effects on everyone. But let’s get to the part about athletic performance: The link between how well you sleep and how well you perform is well-established. Take a deep dive into the study with this insightful paper by Fullagar et.al., 2015.
Moreover, a reduction in sleep quality and quantity could result in autonomic nervous system imbalance, simulating symptoms of overtraining. Increases in pro-inflammatory cytokines (cell signals) following sleep loss could also promote immune system dysfunction and severely hinder your recovery.
Several pieces of evidence in the context of diabetes research have shown a direct link between sleep quality and glucose control. In particular, those with bad glucose control (less stable, more frequent high glucose levels, and more frequent low glucose levels) have poorer sleep compared with those who have better glucose control throughout their day.
People with poorly controlled glucose levels display shorter sleep duration and worse sleep quality, demonstrated by both self-report and objective measures. But despite the studied population of people living with diabetes, it's also been found that glucose dysregulation in sleep frequently happens in those living without diabetes.
So clearly, sleep is crucial for health and performance. But interestingly, glucose and sleep look to have a bidirectional influence on each other. So sleep impacts your glucose but your glucose control impacts your sleep too.
Want to learn how to improve your glucose levels to better optimize sleep? Check out our article 5 Ways to Improve Sleep Quality with CGM and Your Glucose Levels.
How do circadian rhythms relate to glucose metabolism?
Glucose tolerance refers to the ability to dispose of a glucose load or more practically, to metabolize exogenous (ingested) carbohydrates, returning to a baseline glucose level. Or said more simply: The ability to get back to normal after eating some glucose.
Glucose tolerance (your ability to use or store glucose – low glucose tolerance will show larger rushes for the same amount of glucose) has a circadian rhythm to it, and is typically highest in the morning and lowest in the middle of the night. Part of this variation is due to changes in insulin sensitivity (the dose of insulin taken to lower glucose levels by a certain amount).
This shift in metabolism is ascribed to both decreased insulin sensitivity of the muscle and reduced responsiveness of insulin-producing cells in the evening.
To sum it up, the deterioration of glucose tolerance during the day appears to result from both impaired insulin secretion and impaired insulin action later in the day. So glucose response to the same carbohydrate load will usually be lowest in the morning and highest in the evening. But as Supersapiens users know, there are some things you can do to limit your glucose response like a walk post meal for example.
What role does exercise play in “correcting” circadian rhythm shifts?
The phase of the circadian rhythm, both centrally in the brain and peripherally in organs, shifts in response to exercise. Evidence is emerging that exercising at specific times of the day can correct a “misalignment” of the body’s internal clock.
But such relationships can be highly variable between people. In addition, training enhances glucose disposal independent of insulin in the muscle, promoting a lower glucose levels toward the night despite the natural reduction in insulin sensitivity.
So while it may be uncertain that exercise will help correct your circadian rhythm, it is fairly clear that it will improve your glucose response to a meal.
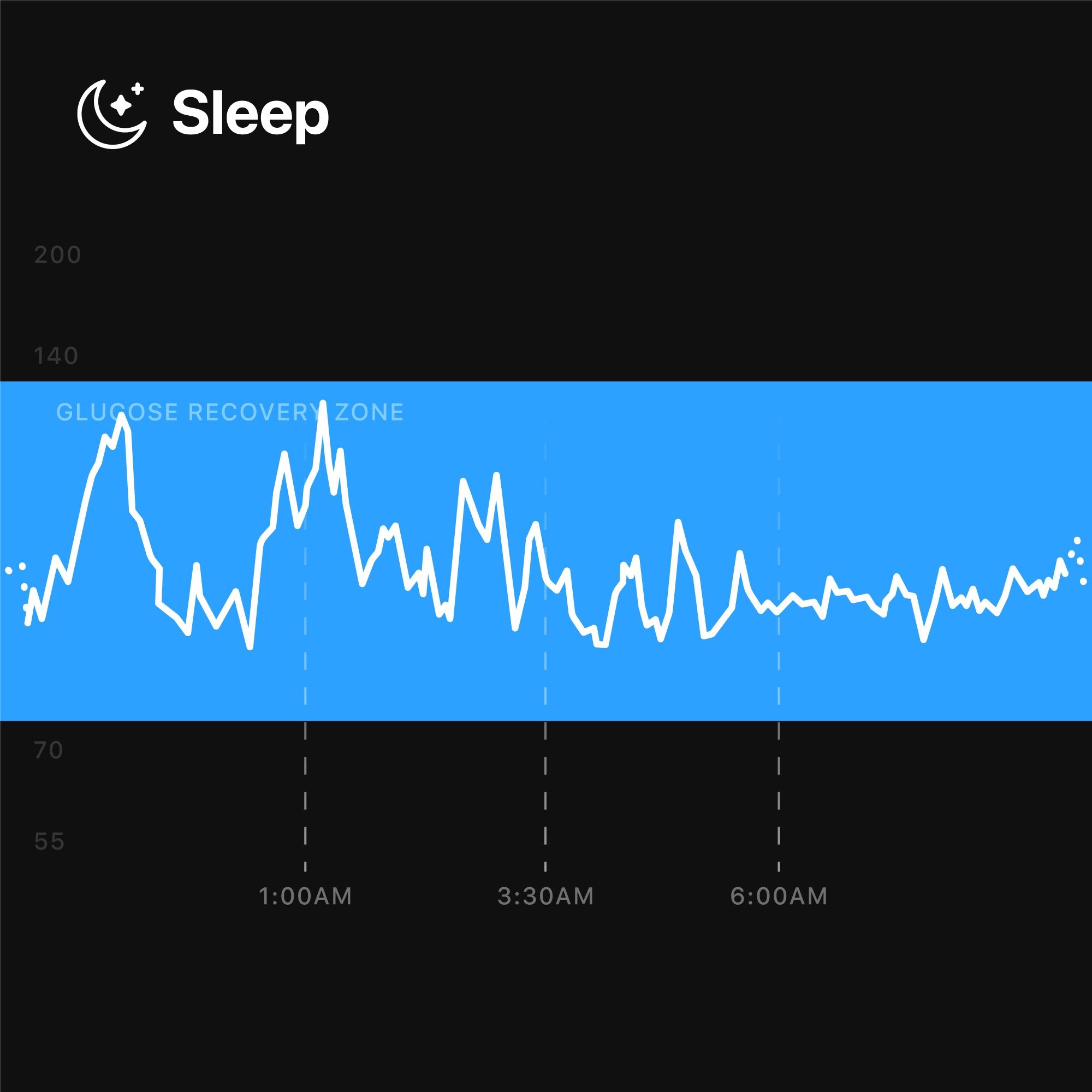
What happens to glucose patterns during sleep?
Glucose usage is highest when we’re awake and almost always lower overnight. Our data shows that, on average, overnight glucose levels are usually 15% lower than during the day and more stable, across a large number of athletes. Broadly, across a night, glucose levels are increased by an average of 20% in the early part of the night, normalizing by the time of waking.
Glucose usage seems to be lowest in non-REM sleep phases, brain metabolism of glucose declines by approximately 11% during Non-REM sleep. But during REM sleep, did you know the brain (which runs predominantly on glucose) is actually very metabolically active? Which could explain variations in the uptake of glucose during such phases of sleep.
During REM sleep, interstitial glucose measures can decrease by as much as 20%, which probably indicates and reinforces the increased uptake and usage by the brain as previously mentioned. (Note: glucose in the interstitial fluid and blood glucose are different. Check out our article to learn more about the relevance of measuring glucose in the interstitial fluid).
So what happens with abnormal circadian rhythms and glucose metabolism?
Even one night of partial sleep deprivation seems to decrease glucose tolerance and insulin sensitivity significantly. This is true of total sleep duration, but looks like it may be specifically and more sensitively related to slow wave sleep, a phase of sleep traditionally associated with more physically restorative processes.
Therefore, there is some suggestion that there may be a causative aspect to the dual association of impaired sleep, particularly deeper phases of sleep, and impaired glucose metabolism. Taken together, the effects of the circadian rhythm and of sleep deprivation, will likely impair your body’s ability to cope with carbohydrates loads.
And what does this mean for you?
Aside from the obvious need to prioritize sleep–with all its benefits to both our health and athletic performance it means you should be ensuring to be extra mindful on days where you have had poor sleep. See the advice on counteracting this below.
And what does this mean for us?
It means we need to have a better understanding of the relationship between sleep quality and glucose control. Asking questions like: What does it mean for our glucose metabolism across days where we’ve had a poor night of sleep? What is the relationship between sleep phases and glucose levels? Can we look at our glucose tolerance (after a meal) and use our daily Average Glucose and our daily rushes (Glucose Stability) as early signs that our body is shifting toward a less favorable biological rhythm?
Due to these potential links, the topic is extremely interesting given glucose levels might also be a good proxy to signal sleep quality or lack of sleep. We will be conducting laboratory and field based research to better explore and understand the mutual relationship between sleep and glucose for athletic performance and longevity.
How can you counteract the effects of sleep loss?
There are a few preliminary steps you can try that may aid you in optimizing your overnight glucose levels so you can identify the correlation of sleep quality with your glucose levels.
- Be more active than normal. This will improve glucose metabolism and potentially impact insulin sensitivity over the short and long term. Taken together, such effects will also improve your glucose tolerance and glucose control overnight.
- Engage in some extensive exercise to ensure you consolidate the benefits of physical activity on glucose control and therefore on sleep. Observe what happens overnight after a resting day or after an exercise day. Note how your body regulates glucose levels overnight depending on the amount of exercise you’ve done that day and what you ate before you went to bed.
- Try to actively work to decrease glucose rushes especially before going to bed; eating to limit glucose rushes and therefore insulin secretion (by changing your food order to eat fibre and fat first before carbohydrates for example) and walking after a meal might improve your overnight glucose control and perceived (or objectified) sleep quality.
Interested in testing this out for yourself? Get your own biosensors at supersapiens.com.
References:
- Allada, Ravi, and Jerome M Siegel. “Unearthing the phylogenetic roots of sleep.” Current biology : CB vol. 18,15 (2008): R670-R679. doi:10.1016/j.cub.2008.06.033
- Frank, Marcos G, and Joel H Benington. “The role of sleep in memory consolidation and brain plasticity: dream or reality?.” The Neuroscientist : a review journal bringing neurobiology, neurology and psychiatry vol. 12,6 (2006): 477-88. doi:10.1177/1073858406293552
- Galambos, Nancy L et al. “Who sleeps best? Longitudinal patterns and covariates of change in sleep quantity, quality, and timing across four university years.” Behavioral sleep medicine vol. 11,1 (2013): 8-22. doi:10.1080/15402002.2011.596234
- Short, Michelle A et al. “The impact of sleep on adolescent depressed mood, alertness and academic performance.” Journal of adolescence vol. 36,6 (2013): 1025-33. doi:10.1016/j.adolescence.2013.08.007
- Fullagar, Hugh H K et al. “Sleep and athletic performance: the effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise.” Sports medicine (Auckland, N.Z.) vol. 45,2 (2015): 161-86. doi:10.1007/s40279-014-0260-0
- Turner, Sara L et al. “Variations in Daily Sleep Quality and Type 1 Diabetes Management in Late Adolescents.” Journal of pediatric psychology vol. 41,6 (2016): 661-9. doi:10.1093/jpepsy/jsw010
- Barone, Mark T U, and Luiz Menna-Barreto. “Diabetes and sleep: a complex cause-and-effect relationship.” Diabetes research and clinical practice vol. 91,2 (2011): 129-37. doi:10.1016/j.diabres.2010.07.01
- Hall, Heather et al. “Glucotypes reveal new patterns of glucose dysregulation.” PLoS biology vol. 16,7 e2005143. 24 Jul. 2018, doi:10.1371/journal.pbio.2005143
- Donga, E., van Dijk, M., van Dijk, J. G., Biermasz, N. R., Lammers, G.-J., van Kralingen, K. W., Corssmit, E. P. M., & Romijn, J. A. (2010). A Single Night of Partial Sleep Deprivation Induces Insulin Resistance in Multiple Metabolic Pathways in Healthy Subjects. The Journal of Clinical Endocrinology & Metabolism, 95(6), 2963–2968. https://pubmed.ncbi.nlm.nih.gov/20371664/
- Knutson KL. Impact of sleep and sleep loss on glucose homeostasis and appetite regulation. Sleep Med Clin. 2007 Jun;2(2):187-197. doi: 10.1016/j.jsmc.2007.03.004. PMID: 18516218; PMCID: PMC2084401.
- Basse, Astrid L et al. “Skeletal Muscle Insulin Sensitivity Show Circadian Rhythmicity Which Is Independent of Exercise Training Status.” Frontiers in physiology vol. 9 1198. 28 Aug. 2018, doi:10.3389/fphys.2018.01198
- Van Cauter, E., Blackman, J. D., Roland, D., Spire, J. P., Refetoff, S., & Polonsky, K. S. (1991). Modulation of glucose regulation and insulin secretion by circadian rhythmicity and sleep. Journal of Clinical Investigation, 88(3), 934–942. https://pubmed.ncbi.nlm.nih.gov/1885778/
- Wolff, G., and Esser, K. A. (2012). Scheduled exercise phase shifts the circadian clock in skeletal muscle. Med. Sci. Sports Exerc. 44, 1663–1670. doi: 10.1249/MSS.0b013e318255cf4c
- Schroeder, A. M., Truong, D., Loh, D. H., Jordan, M. C., Roos, K. P., and Colwell, C. S. (2012). Voluntary scheduled exercise alters diurnal rhythms of behaviour, physiology and gene expression in wild-type and vasoactive intestinal peptide- deficient mice. J. Physiol. 590, 6213–6226. doi: 10.1113/jphysiol.2012.233676
- Bialasiewicz P, Pawlowski M, Nowak D, Loba J, Czupryniak L. Decreasing concentration of interstitial glucose in REM sleep in subjects with normal glucose tolerance. Diabet Med. 2009 Apr;26(4):339-44. doi: 10.1111/j.1464-5491.2009.02684.x. PMID: 19388962.
- Buxton OM, Pavlova M, Reid EW, Wang W, Simonson DC, Adler GK. Sleep restriction for 1 week reduces insulin sensitivity in healthy men. Diabetes. 2010 Sep;59(9):2126-33. doi: 10.2337/db09-0699. Epub 2010 Jun 28. PMID: 20585000; PMCID: PMC2927933.
- Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999 Oct 23;354(9188):1435-9. doi: 10.1016/S0140-6736(99)01376-8. PMID: 10543671.
- Tasali E, Leproult R, Ehrmann DA, Van Cauter E. Slow-wave sleep and the risk of type 2 diabetes in humans. Proc Natl Acad Sci U S A. 2008 Jan 22;105(3):1044-9. doi: 10.1073/pnas.0706446105. Epub 2008 Jan 2. PMID: 18172212; PMCID: PMC2242689.
